BCBST News Center, Jesse Thompson, Jan. 26, 2021
Key Takeaways
- COVID-19 disproportionately affects communities of color across the country, and especially in Tennessee.
- BlueCross has created its own Social Vulnerabilities Index to identify and support individuals who are at greater risk for health issues, including those more susceptible to a COVID-19 diagnosis.
- The BlueCross Foundation has awarded Nashville’s Meharry Medical College a $325,000 grant to address vaccine hesitancy within minority populations through education and access to health care resources.
COVID-19 continues to challenge and threaten all Americans. But we’re learning more about its far-reaching effect on Tennesseans and our communities.
For example, COVID-19 has disproportionately affected minority communities and resulted in more infections, hospitalizations and deaths, mainly due to social vulnerability.
“Social vulnerability refers to a community’s ability to withstand external impacts to health,” says Dr. Andrea Willis, BlueCross chief medical officer. “In other words, it evaluates how outside forces like disasters or disease outbreaks compound the odds already stacked against these communities. If the totality of those odds are too high, it leaves very little opportunity for that community to overcome them — and even less opportunity to win an uneven fight.”
To address these vulnerabilities, BlueCross has partnered with Nashville’s Meharry Medical College, the largest private historically Black academic health sciences center in the United States, dedicated to educating health care professionals and scientists.
The first phase of our partnership aims to better understand potential disparities in acceptance of the COVID-19 vaccines, and to raise awareness now that safe and effective vaccines are being distributed. To support this effort, the BlueCross Foundation has issued a $325,000 grant to Meharry aimed at examining social determinants of health, improving understanding of COVID-19 disparities, and finding ways to address their influence on COVID-19 vaccine hesitancy.
 Through this grant, Meharry and BlueCross will be able to identify those at the greatest risk for remaining unvaccinated and specific populations who may benefit most from vaccination.
Through this grant, Meharry and BlueCross will be able to identify those at the greatest risk for remaining unvaccinated and specific populations who may benefit most from vaccination.
“Our partnership with Meharry focuses on evaluating and identifying populations that may be hesitant to receive a COVID-19 vaccine, even after clinical trials, FDA approval and the start of phased distribution,” Dr. Willis says. “The SVI will also be leveraged in the build-out of a COVID-19 Vaccine Hesitancy Index. We’re confident our collaboration will provide more insightful data into the mistrust between minority populations and the health care system.”
Meharry has been on the frontlines of addressing COVID-19 from all avenues, from leading assessment sites to vaccine trials to raising vaccine awareness.
“There is clear evidence demonstrating health disparities associated with COVID-19 — cases, hospitalizations, death — and vaccine hesitancy,” says Dr. Bryan Heckman, director, Center for the Study of Social Determinants of Health, and associate professor, Psychiatry and Behavioral Sciences, at Meharry. “If left unaddressed, we have concerns this could compound or elongate this unfortunate reality and leave behind underserved populations.”
“By examining drivers of vaccine hesitancy, we hope to mitigate disparities and optimize health equity.”
Social determinants drive health inequalities and disparities
According to the Kaiser Family Health Foundation, social determinants are “the conditions in which people are born, grow, live, work and age that shape health.” These can include education, access to health care, income, among others, and are linked to a lack of opportunity and resources to protect and improve health. They’re also most responsible for health inequalities, the unfair and avoidable differences in health status seen with and between populations.
Pre-existing conditions like diabetes, cardiovascular disease, and obesity occur more often in minority populations and are amplified by inequalities, resulting in increased percentages of severe COVID-19 cases.
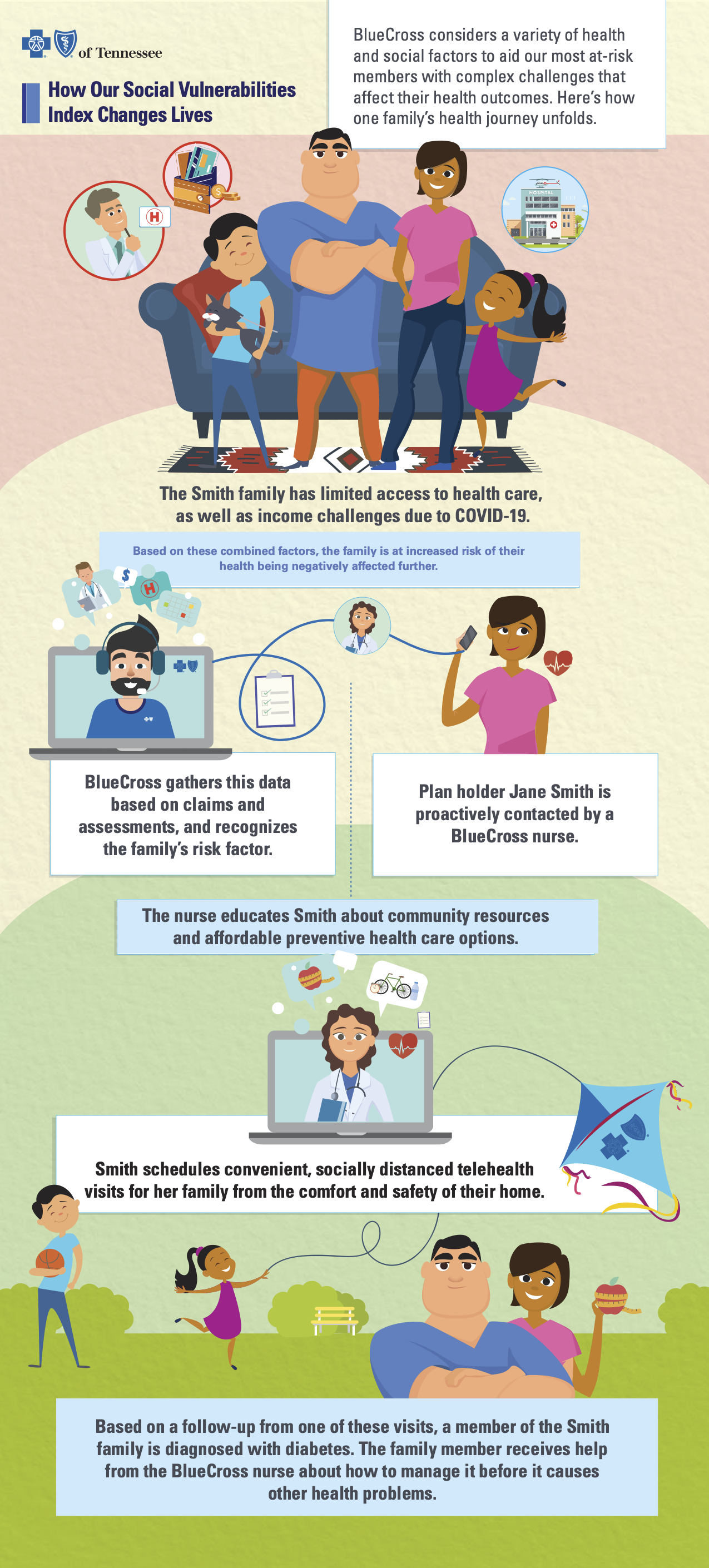
To better understand the role of social determinants of health, BlueCross developed a Social Vulnerabilities Index (SVI).
“The determinants we incorporated to build the SVI include transportation, language, education, and housing, to name a few,” says Sherri Zink, chief data engagement officer at BlueCross. “As the number of social vulnerabilities goes up for an individual, so does their score.”
The SVI is designed to serve everyone with any of those 19 factors, regardless of whether they’ve received a positive COVID-19 diagnosis. We envision it will be used to help identify and engage with vulnerable populations to remove barriers to care.
An aggregate score that ranges from 0 to 19, the SVI quantifies the number of social determinants for which a member may be at risk. A higher score indicates increased exposure to vulnerabilities that may negatively affect health.
How we use the SVI
We put the SVI into practice by looking at a member’s overall health journey and assigning them an index level at low, moderate, or high-risk.
Our research shows that while we see more complications occurring across all populations at older ages, we see complications in earlier age brackets for Black and Hispanic communities.
“For BlueCross members visiting doctor’s offices and hospitals across the state, a larger number of people getting tested for COVID-19 are in the 21-40 age category,” Sherri says. “Looking at our Hispanic members, 44% who are tested fall in the 21-40 age category — and 46% test positive.”
Hospitalizations tell a very different story, as they’re more prevalent among younger age groups in the Hispanic and the Black populations. Of our members, 30% of Hispanics age 21-40 that test positive for COVID-19 are hospitalized, compared to 26% Black and 9% White.
These results highlight that one size of care doesn’t fit all, and our members are affected and access health care differently.
For those diagnosed with COVID-19, even with their insurers covering the cost of treatment, ER visits and hospitalizations resulted in longer and costlier overall journeys. This is due to the greater number of social determinants, harsher symptoms and lengthier recoveries at play. Those journeys in turn create more of those 19 factors, and a higher-than-average social vulnerability score.
Download a copy of our infographic.
Our data shows that fewer social vulnerabilities mean a lower cost of care and a positive overall health impact. More importantly, when people are healthier and experience less stress from financial burden, they can enjoy a better quality of life.
“Vulnerabilities vary by ethnic group, and mapping health care journeys give us insights into different experiences, complexities, and patterns of treatment,” Sherri says. “We know people have different risk factors, and different things happen throughout their journeys. The SVI gives us insight into social vulnerabilities that may impact medical events and highlights those areas where we may have an opportunity to intervene and be more proactive in raising awareness in these populations.”
Our nurses’ and other clinical experts’ daily work with our members make these interventions possible. Our care coordinators and health navigators can see the score severity and the vulnerabilities that make up the score. For our Medicaid members, the SVI is linked to a community resource database that alerts care coordinators to available community resources to address those vulnerabilities.
The SVI is just one way we’re working to address vulnerabilities and health care inequality. In addition, the BlueCross Foundation has given nearly $5 million to our communities during the pandemic and engaged in a variety of efforts to improve their health, including:
- Funding COVID-19 testing for uninsured and underinsured populations
- Supporting education through increased broadband access for students and six diversity scholarships for students pursuing health care professions
- Building BlueCross Healthy Places for communities needing well-designed spaces for all to engage in physical activity
- Launching a flu awareness campaign to encourage all Tennesseans to get flu shots; especially important this flu season with COVID-19 compromising the environment
In conjunction with Meharry, we’ll develop strategies to enhance awareness and improve trust in the health care system, thereby reducing barriers to care. We plan to expand our partnership to raise awareness of social determinants of health in the health care and minority communities to combat inequality in care delivery.
“We can also focus and tailor efforts to vulnerable populations at greatest risk for chronic kidney disease, diabetes, hypertension, asthma, obesity, etc.,” Dr. Heckman says. “Our research will help uncover the best approach to providing resources and optimizing health equity.”
Adds Dr. Willis, “While the data tells a story, the involvement of all of the stakeholders is what dictates how the story progresses, and ultimately, how it ends.”
